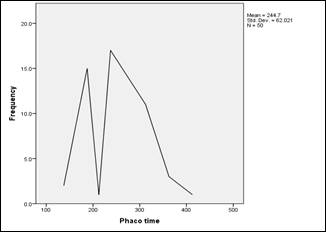
Fig. 1: Mean Phacoemulsification time
≤6/60 (≤
0.1) to 6/6 (1.0) (Table 3). BCVA was significantly higher than mean preoperative
BCVA.
(P < 0.001).
DISCUSSION
Mature and hypermature cataracts constitute
a significant volume of the cataract surgical load in ophthalmic practice in
the developing countries. There were an estimated 1,140,000 (962,000-1,330,000)
blind adults in Pakistan in 2003. Countryside areas had a higher frequency of
blindness than did urban areas (3.8% vs. 2.5%). Most patients have advanced
stages of cataract with intumescent, mature or hypermature cataract. Majority
of these patients are less privileged8.
White mature cataracts are a challenge for
cataract surgeon and carry some difficulties. The most critical step of phacoemulsification
surgery is Continuous Curvilinear Capsulorhexis. If it is not complete, some
intraoperative complications such as posterior capsule rupture, vitreous loss
and nucleus drop may occur. Because the red reflex is compromised in white
cataract, it is difficult to complete CCC safely. Trypan blue provides a safe
CCC7,9.
General recommendations for visualization
of anterior capsule in eyes with mature white cataract include dimming the
operation room lights, increasing the magnification of microscope, using
oblique illumination, capsule dyes. Giammaria D et al and Wong et al, stained
the capsule under an air bubble, it was reported that using the dye under the
dispersive viscoelastic material was easier and safe. The air bubble technique
was reported to be time consuming7,10. The rate of conversion to
ECCE in white cataracts as a result of an incomplete CCC has been as low as 3.85%
when Trypan blue is used compared to 28.3% when no staining was used. In our
study, we used Trypan blue in all patients, and radial tears occurred in five
patients and rate of conversion to ECCE was 10%. It has been reported that Trypan
blue did not cause any inflammation, corneal edema, corneal thickening, decrease
in endothelial cell count and IOP rise11. Portes et al demonstrated
that Trypan blue caused lens epithelial cell death, which supported the
hypothesis that staining with Trypan blue 0.1% helps reducing the incidence of
posterior capsule opacification after cataract surgery. The frequency of
capsular rupture and vitreous loss can be reduced by staining the anterior
capsule with the Trypan blue to identify the capsular tear at an early stage.
We achieved a 5 mm capsulorhexis in most of the cases 12.
Kara junior et al recommended the mini
rhexis technique for white intumescent cataracts in which primarily a small CCC
was performed then enlarged. Two stages CCC prevented unanticipated radial
tears of the initial capsulotomy due to elevated intra capsular pressure13.
We aspirated liquefied milky cortical matter via cannula in 15 patients before
finishing CCC to avoid sudden radial tears due to highly intracapsular
pressure. Chen and Wu suggested automated irrigation and aspiration by lowering
of BSS bottle to aspirate the liquefied milky lens contents before
phacomulsification14. Daglioglu et al suggested an innovative
capsulorhexis technique in white cataract surgery in which CCC was completed by
using an irrigation and aspiration system by phaco machine, it was found safe
in white cataracts15.
Although hydro dissection was not
recommended in white mature cataracts, we observed that gentle hydro dissection
broke the cortico-capsular adhesions that could resist free nucleus rotation1.
Singh et al reported cortico-capsular adhesions resulted in different nucleus
rotation in brunescent and black cataracts. Nucleus rotation is critical for
phacoemulsification16.
Posterior capsule is not only weak but also
flaccid with wrinkles and laxity that makes it prone to be ruptured. The
problem is worsened by absence of any epinucleus that protects the posterior
capsule. A useful step is to inject a dispersive non–cohesive viscoelastic
behind the nucleus during the phacoemulsification, which will provide an
artificial epinucleus to keep the posterior capsule back from the operating
plane and stabilize the nucleus against tumbling17.
In Brunescent and black cataracts, the lens
fibers were found to be very cohesive thus making division difficult. White
cataracts in our study were usually brittle and not very hard; they were safely
divided and emulsified. During the division and aspiration of the nucleus, edge
of the hard nucleus may cut the posterior capsule, resulting in rupture; also
radial tears in anterior capsulotomy may extend to posterior capsule and cause
rupture. Therefore, the incidence of posterior capsule rupture is higher in
mature cataracts18. In our study rate of posterior capsular rupture
was 6%.
Phacoemulsification of hard nucleus
requires higher ultrasonic energy, which is partially converted to heat energy
causing corneal endothelial damage and corneal burns. Fluid dynamics during
phacoemulsification may cause endothelial cell damage if it lasts longer18.
With aging, endothelial cell count decreases, this is another risk for patients
with mature cataracts; therefore, chances of post-operative corneal edema is
higher in patients with mature cataract18,19.
In our study, we did not encounter
complications of capsular fibrosis and geometrical decentration. In another study,
capsular fibrosis was reported to occur in 12% of eyes with white mature
cataracts all of which had a capsulorhexis diameter of less than 5 mm20.
Small capsulorhexis leads to capsule contraction.
Yuan et al recommended that ophthalmic
viscosurgical device assisted sutureless cataract surgery, usually without
additional instruments, or sutures presented an efficient and uncomplicated
technique for managing a brunescent or mature cataract21. Venkatesh
et al compared manual small incision cataract surgery with phacoemulsification
for white cataract and reported that both techniques achieved excellent visual
outcomes with low complication rates22. Wong et al suggested that
micro-incisional cataract surgery with bimanual phacoemulsification appeared to
be a hopeful alternative for management of white cataracts23. Kim
and Jang proposed drill and chop technique for hard cataracts, which required
complete engagement of central nucleus by phaco tip. First, a hole was drilled
into the endonucleus by rotating the Kelman phaco tip clockwise, nucleus was
deeply impaled horizontally and completely engaged by phaco tip followed by
vertical chopping and it resulted safer and more effective vertical chopping in
patients with harder cataracts24. Li et al described the peripheral
radial chop technique in phacoemulsification of harder nuclei and stated that
it was effective without grave complications in hands of skilled surgeons25.
The limitation of our study was that it was performed in one
center. More studies need to be performed with larger number of patients in
multiple centers.
CONCLUSION
White mature cataract is
a challenge for phaco surgeons but with appropriate techniques such as two
stage capsulorhexis and use of additional capsule staining dyes can achieve
excellent visual outcomes and low complication rates.
REFERENCES
1.
Ermisş SS, Oztürk F, Inan UU. Comparing the efficacy and safety of phacoemulsification in white
mature and other types of senile cataracts. Br J Ophthalmol. 2003 Nov;
87(11):1356-9.
2.
Khan AQ, Qureshi B, Khan D. Rapid assessment of cataract blindness in age 40 years and above
in district skardu, Baltistan, Northern areas, Pakistan. Pak J Ophthalmol.
2003; 19: 84-9.
3.
Ilavska M, Kardos L.
Phacoemulsification of mature and hard nuclear cataracts. Bratisl Lek Listy, 2010;
111 (2): 93-6.
4.
Susic N, Brajkovic J, Susic E, Kalauz-Surac I. Phacoemulsification in eyes with white cataract. Acta Clin Croat, 2010;
49 (3): 343-5.
5.
Hawlina M, Stunf S, Hvala A. Ultrastructure of anterior lens capsule of intumescent White
cataract. Acta Ophthalmol. 2011; 89 (4): e367-70.
6.
LoBue SA, Tailor P, LoBue TD. A Simple, Novel Approach to Capsulorhexis Formation in the Setting
of A Mature Cataract and Miotic Pupil. Clin Ophthalmol. 2019 Dec 2; 13: 2361-2367.
7.
Giammaria D, Gianotti M, Scopelliti A, Pellegrini G, Gianotti B. Under-air staining of the anterior capsule using trypan blue with
a 30 G needle. Clin Ophthalmol. 2013; 7: 233-235.
8.
Jadoon MZ, Dineen B, Bourne RR, Shah SP, Khan MA, Johnson GJ, et
al. Prevalence of blindness and
visual impairment in Pakistan: The Pakistan National Blindness and Visual
Impairment Survey. Invest Ophthalmol. 2006; 11: 4749-55.
9.
Rossiter J, Morris A.
Trypan blue vital staining of the anterior lens capsule in the management of
cataract in true exfoliation of the lens capsule. Eye, 2005; 19: 809-10.
10.
Wong VW, Lai TY, Lee GK, Lam PT, Lam DS. A prospective study on trypan blue capsule staining under air vs
under viscoelastic. Eye (Lond.), 2006; 20 (7): 820-825.
11.
Cheour M, Ben Biahim F, Zauad A. Trypan blue capsule staining for phacoemulsification in white
cataract. J Fr Ophthalmol. 2007; 30 (9): 914-917.
12.
Portes AL, Almeida AC, Allodi S, Monteiro ML, Miguel NC. Trypan Blue Staining for Capsulorhexis; ultrastructural effect on
lens epithelial cells and capsules. J Cataract Refract Surg. 2010; 36 (4) 582-7.
13.
Kara-Junior N, de Santhiago MR, Kawakami A, Caricondo P, Hidaet
WT. Mini-rhexis For White
Intumescent Cataracts. Clinics (sao Paulo). 2009; 64 (4): 309-312.
14.
Chen YJ, Wu PC.
Automated irrigation/aspiration before phacoemulsification in eyes with white
cataracts. Ophthalmic Surg Lasers Imaging, 2005; 36 (2): 118-21.
15.
Daglioglue MC, Coskun M, Ilhan O, Tuzco EA, Ilhan N, Ayintap E, et
al. A novel capsulorhexis
technique in white cataract surgery. Semin Ophthalmol. 2014; 30 (4): 264-267.
16.
Singh R, Vasavada A, Janaswamy G. Phacoemulsification of Brunescent and black cataracts. J Cataract
Refract Surg. 2001; 27: 1762-9.
17.
Cetinkaya S, Gurdag T, Akcam N. Phacoemulsification in eyes with white mature cataract. Sch. J. App.
Med. Sci. 2015; 3 (2c): 701-4.
18.
Bilgin B, Eltutar K, Sezgin BI. Comparison of phacoemulsification results of mature and
nucleocortical cataracts. Turk J Ophthalmol. 2006; 36: 219-22.
19.
Sizmaz S, Peli A, Yaycioglu RA. The use of trypan blue in patients with white cataract. Turk J
Ophthalmol. 2007; 37: 178-181.
20.
Shahid E, Sheikh A, Fasih U. Complications of hypermature cataract and its visual outcome. Pak
J Ophthalmol. 2011; 27 (2): 58-62.
21.
Yuan X, Song H, Hua X. Ophthalmic viscosurgical device- assisted sutureless-incision
cataract surgery for a hard nucleus or mature cataract. J Cataract Refract
Surg. 2014; 40 (4): 517-20.
22.
Venkatesh R, Tan CS, Sengupta S, Ravindran RD, Krishan KT, Chang
DF. Phacoemulsification versus
manual small incision cataract surgery for white cataract. J Cataract Refract
Surg. 2010; 36 (11): 1849-54.
23.
Wong VW, Lai TY, Lee GK. Safety and efficacy of micro-incisional cataract surgery with
bimanual phacoemulsification for white mature cataract. Ophthalmologica. 2007; 221
(1): 24-8.
24.
Kim DY, Jang JH.
Drill and chop: modified vertical chop technique for hard cataract. Ophthalmic
Surg Lasers Imaging, 2012; 43 (2): 169-72.
25.
Li SW, Xie LX, Song ZH. Peripheral radial chop technique for phacoemulsification of hard
cataracts. Chin Med J (Engl.). 2007; 120 (4): 284-86.